Health Check
In order to raise the standard of operational hospital buildings, a holistic approach must be taken, writes Cundall’s Amin Azarmi.
When standards change there are two typical ways to respond. First, scramble to do the minimum required to comply. Or second, take the opportunity to improve overall building performance while also addressing enhanced regulatory requirements.
The introduction of the new AS 4187 Standard for Australian hospitals is one such case in point.
On the surface, it sets out straightforward requirements around managing and tracking contaminated equipment. But – and it’s a big but – there’s a whole series of factors involved in ensuring that items such as a used surgical tool do not create an infection risk for staff or patients in other parts of the hospital.
Addressing those factors can open up possibilities for stepping up to a whole new set of policy and market valuation standards around building performance, energy-efficiency and the trajectory to all-electric net zero assets.
Raising the standard of hospital building performance can involve:
- Implementing energy-efficient systems
- Using sustainable building materials
- Optimising indoor air quality
- Providing adequate daylight and views
- Ensuring proper ventilation
- Incorporating infection control measures.
Additionally, it can involve designing spaces that promote healing, patient comfort, and staff well-being, as well as providing flexibility to accommodate future changes in healthcare delivery. Regular maintenance and monitoring of building systems can also help ensure long-term performance and cost savings.
“It can involve designing spaces that promote healing, patient comfort, and staff well-being, as well as providing flexibility”
AS-4187 compliance and opportunities
Compliance with AS/NZS 4187 can provide opportunities to improve hospital building performance in several ways.
Firstly, the standard requires the regular monitoring and testing of HVAC (heating, ventilation and air conditioning) systems to ensure they are functioning effectively and providing the necessary levels of air quality and ventilation. By implementing a comprehensive monitoring and maintenance program, hospitals can identify and address issues with their HVAC systems such as leaks or inefficient operation, which can result in energy waste and decreased performance.
Secondly, the requirement for specialised ventilation systems in sterilisation areas can be an opportunity to implement energy-efficient technologies, such as heat-recovery ventilation systems or demand-controlled ventilation, which can improve energy efficiency while still meeting AS/NZS 4187 requirements.
Thirdly, compliance with AS/NZS 4187 can provide an opportunity to improve the overall indoor air quality and infection control of a hospital facility, which can benefit both patients and staff. This can include implementing advanced air filtration and purification systems, improving ventilation rates and air exchange, and optimizing temperature and humidity levels. All of these enhancements can contribute to a healthier and more comfortable indoor environment.
Overall, compliance with AS/NZS 4187 can serve as a catalyst for hospitals to improve their building performance and adopt energy-efficient and sustainable practices, while also improving the quality of care for patients and promoting a healthy and productive work environment for staff.
Space pressurisations for AS-4187 compliance
Positive and negative space pressurisation is an essential aspect of hospital design and construction that helps ensure compliance with AS/NZS 4187 standards for infection control.
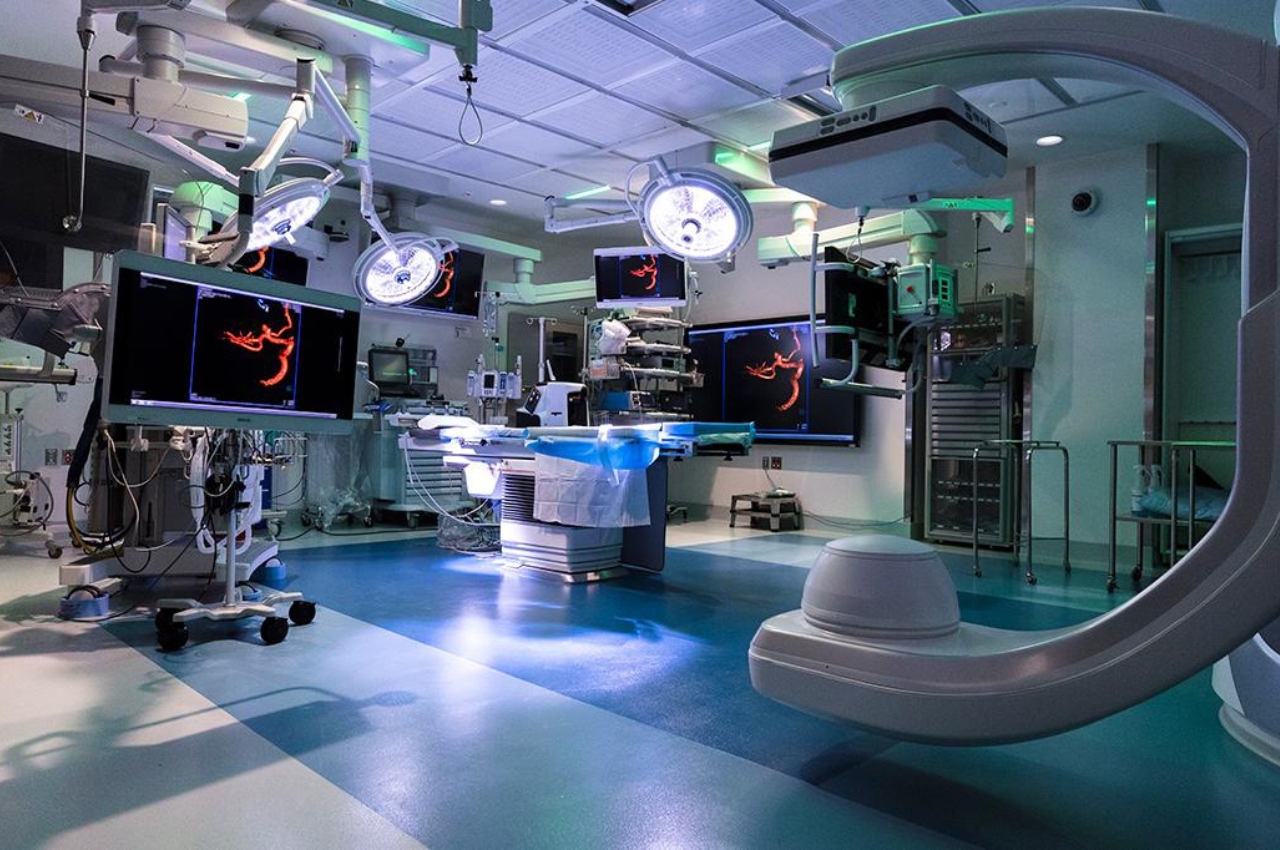
Positive pressure spaces have a higher air pressure than surrounding areas, which prevents airborne contaminants that could cause infections from entering the space. In hospitals, areas that require positive pressure typically include operating rooms, intensive care units, and other sterile areas. Positive pressure helps maintain a clean and sterile environment.
On the other hand, negative pressure spaces have lower air pressure than surrounding areas, which prevents contaminants from leaving the space and spreading to other areas. Areas that require negative pressure in hospitals include isolation rooms, where patients with contagious diseases are treated, or in emergency rooms where patients with respiratory infections may be treated. Negative pressure helps prevent the spread of airborne contaminants and protect other patients and staff in the hospital.
To comply with AS/NZS 4187 standards, hospitals must properly manage the pressurisation of different areas of the hospital. This may involve the installation of specialised HVAC systems, or introducing airlocks or anterooms that help control the flow of air between spaces and maintains appropriate levels of pressure.
AS/NZS 4187 compliance also requires hospitals to establish a comprehensive air monitoring and maintenance program to ensure HVAC systems are functioning effectively and providing the necessary levels of air quality and ventilation.
“Compliance with AS/NZS 4187 can provide an opportunity to improve the overall indoor air quality and infection control of a hospital facility”
Pressurisation system design
Positive and negative pressurisation can be achieved using both variable air volume (VAV) and constant air volume (CAV) systems, although there are some differences in their implementation.
CAV system:
- Positive pressurisation: In a CAV system, positive pressurisation can be achieved by supplying a constant volume of air to a space, ensuring that the supply airflow rate is higher than the exhaust airflow rate.
- Negative pressurisation: Negative pressurisation in a CAV system is achieved by exhausting a higher volume of air from a space compared to the supply airflow rate.
VAV system:
- Positive pressurisation: In a VAV system, positive pressurisation can be achieved by supplying more air to a space than is exhausted, resulting in a slightly higher pressure in the space compared to surrounding areas. This is typically achieved by adjusting the VAV terminal boxes to deliver a higher volume of supply air to the space.
- Negative pressurisation: Similarly, negative pressurisation can be achieved in a VAV system by exhausting more air from a space than is supplied. This is typically accomplished by adjusting the VAV terminal boxes to deliver a lower volume of supply air to the space or by increasing the exhaust airflow rate.
It’s important to note that while VAV and CAV systems can both be used to achieve positive and negative pressurisation, VAV systems offer more flexibility in terms of controlling and adjusting airflow rates based on space requirements. VAV systems can modulate the airflow based on room pressure, temperature, occupancy, or other factors, allowing for more precise control and energy efficiency.
VAV systems can respond, and fluctuate, in real time to actual conditions. So, if for example a room has not been entered for several hours and the pressure is stable at the optimum level, the AHUs can reduce airflow so long as pressure is being maintained. When the door is opened or during busy periods, AHUs can automatically ramp up to ensure the appropriate level is present.
With the correct set-up and commissioning, VAV systems are extremely energy-efficient, because they can be tuned to respond precisely to actual conditions, rather than pre-set to predicted conditions. This also enables temperature to be managed according to real-time conditions, which is where some major energy savings can be achieved.
There are also new pressure-stabilisation dampers with smart controls that can fine-tune the rate of air delivery in response to the pressure data received from sensors. This is a far more simplified method and precise approach than the somewhat blunt instrument of set points that were previously the solution.
CAV systems are relatively simpler in design and operation, making them easier to install and maintain, and typically have lower upfront costs due to simpler equipment and controls. CAV systems supply a constant airflow regardless of the space pressure, heating or cooling demand, which can lead to energy wastage during periods of partial load or low demand. CAV systems also may not adjust airflow rates based on occupancy or air quality, potentially leading to inadequate ventilation in some areas.
Ultimately, the choice between VAV and CAV systems for achieving positive and negative pressurisation depends on the specific requirements of the building, the level of control needed, and the desired energy efficiency goals.
“Overall, compliance with AS/NZS 4187 can serve as a catalyst for hospitals to improve their building performance and adopt energy-efficient and sustainable practices”
Smart building services for healthcare to improve the indoor air quality
Smart building services for healthcare can be utilised to improve indoor air quality by monitoring and controlling various factors that impact air quality. This can include deploying sensors and other monitoring devices to track the levels of pollutants such as particulate matter, volatile organic compounds, and carbon dioxide, as well as temperature and humidity levels.
These sensors can be connected to a centralised control system that uses algorithms and AI to adjust ventilation rates and air exchange rates, ensuring optimal air quality throughout the facility. Additionally, smart systems can facilitate the integration of advanced air filtration and purification systems, which can remove airborne pathogens and other contaminants from the air. By maintaining high indoor air quality, healthcare facilities can reduce the risk of infection, promote patient comfort and staff productivity, and support overall health and well-being.
Smart systems for healthcare assets
Smart systems for healthcare assets refer to the use of advanced technologies to improve the management and performance of healthcare facilities and equipment. This can include implementing Internet of Things (IoT) devices, such as sensors and actuators, to monitor and control assets, as well as using data analytics and artificial intelligence (AI) to optimise asset utilisation, maintenance, and replacement.
Smart systems can also facilitate real-time tracking of medical devices and supplies, improve patient safety, and enhance operational efficiency. Additionally, they can support remote patient monitoring and telemedicine, which can help to expand access to care and improve patient outcomes.
“Negative pressure spaces have lower air pressure than surrounding areas, which prevents contaminants from leaving the space and spreading to other areas”
Retrofit for future-fit and taking out the gas
Retrofitting existing hospitals to achieve improved indoor air quality, net-zero energy consumption, compliance with new standards such as AS-4187, and increased staff and patient well-being requires a holistic approach that considers various building systems and operations. Here are some key steps that can be taken to achieve these goals:
- Conduct an energy audit: Start by conducting a thorough energy audit to identify areas of inefficiency and opportunities for improvement. This may include an analysis of the building’s HVAC system, lighting, insulation, and other building systems.
- Upgrade the HVAC system: One of the most important areas to consider in a hospital retrofit is the HVAC system. This may involve upgrading the existing system to improve energy efficiency and air quality, as well as implementing specialised systems, such as airlocks or anterooms, to comply with AS-4187 standards.
- Implement renewable energy sources: Consider implementing renewable energy sources, such as solar or wind power, to reduce the hospital’s reliance on non-renewable energy sources and move towards achieving net-zero energy consumption.
- Improve the building envelope: Improving the building envelope, such as insulation and window systems, can help reduce energy waste and improve indoor air quality
- Install green roofs: Planting vegetation on the roof of a building, can help improve air quality and reduce the urban heat island effect.
- Prioritize staff and patient well-being: Consider implementing features that promote staff and patient well-being, such as biophilic design elements, access to natural light and green space, and healthy food options in the cafeteria.
Overall, retrofitting existing hospitals to achieve these goals is a complex process that requires careful planning and collaboration between hospital staff, building professionals, and other stakeholders.
By taking a holistic approach and considering multiple building systems and operations, hospitals can improve their energy efficiency, indoor air quality, and the overall well-being of staff and patients while reducing their environmental impact.
This article appears in Ecolibrium’s March-April 2024 edition
View the archive of previous editions
Latest edition
See everything from the latest edition of Ecolibrium, AIRAH’s official journal.




